Why Measure TSH in a Patient with Gynecomastia?
Case Vignette:
You are a new endocrinology resident in a tertiary hospital. A 26-year-old man presents to the outpatient clinic with new-onset bilateral gynecomastia. There is no nipple discharge, and both personal and family medical histories are unremarkable. He reports no use of medications or supplements. Laboratory tests have not yet been performed.
During discussion of the case with your supervising endocrinologist, you are asked whether the patient has symptoms or signs of thyroid dysfunction. You admit that you did not assess these symptoms and signs. Your supervisor recommends a laboratory work-up including estradiol, testosterone, LH, beta-hCG, and additionally TSH.
Question: Why is TSH measurement indicated in this patient with gynecomastia?
Gynecomastia may be a sign of thyrotoxicosis resulting from an androgen–estrogen imbalance driven by two primary pathogenic mechanisms: (1) thyroid hormone–induced elevation of hepatic sex hormone–binding globulin (SHBG) production, which reduces the bioavailability of androgens, particularly testosterone; and (2) increased aromatase activity, which enhances the conversion of testosterone to estrogen.
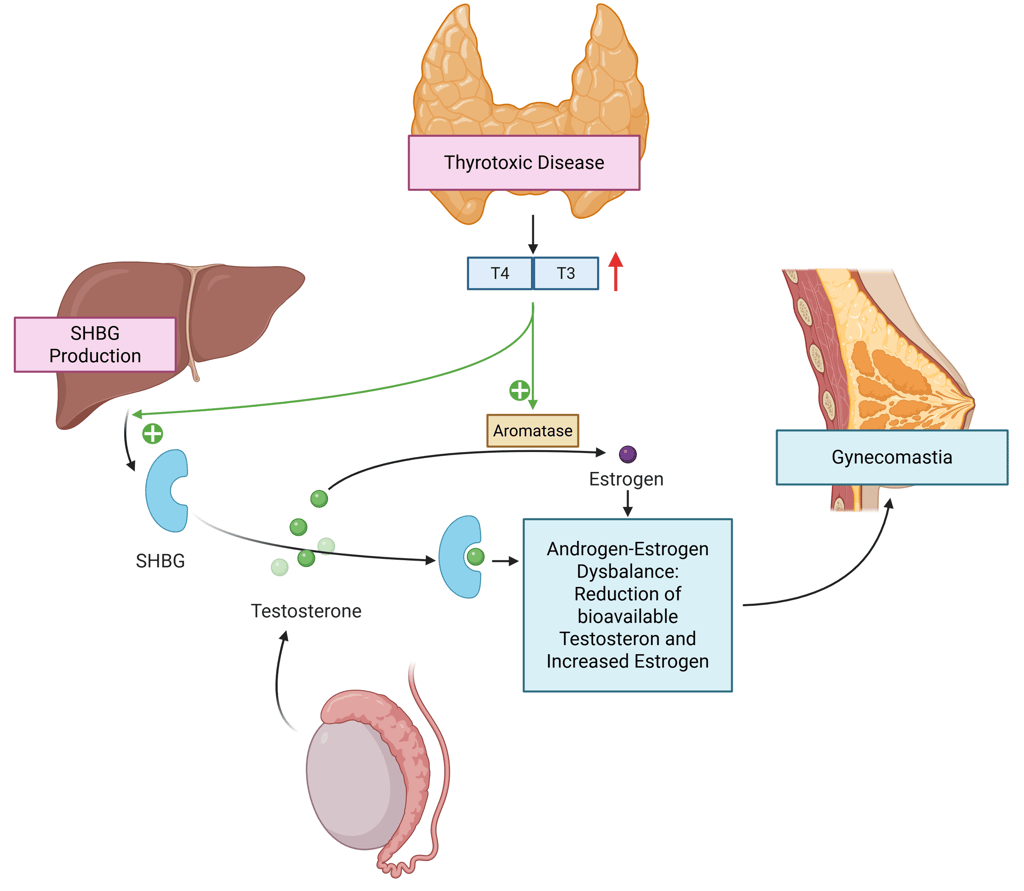
Illustration: Pathomechanisms of thyrotoxicosis causing gynecomastia
Therefore, in patients with thyrotoxicosis, gynecomastia is often accompanied by a slight increase in serum estradiol while LH remains within the normal range. Other characteristic laboratory findings include high-normal or elevated FSH and LH, total testosterone in the high-normal or elevated range, increased levels of sex hormone–binding globulin (SHBG), and reduced or low-normal free testosterone.
Opinions and Guidelines differ regarding TSH measurement in the evaluation of gynecomastia. Some recommend including TSH as part of the initial laboratory work-up for all patients, while others suggest measuring it only if a characteristic biochemical pattern, involving LH, total testosterone, estradiol, and SHBG, is present, or if there are clinical features of thyrotoxicosis. In practice, gynecomastia due to thyroid hormone excess is usually accompanied by clear signs and symptoms of thyrotoxicosis, making the diagnosis often clinically apparent.
Returning to the Case
Further history and examination revealed no symptoms or signs of thyrotoxicosis, and thyroid function tests were entirely normal. On physical examination, the right testis was enlarged. β-hCG was found to be elevated. Urgent testicular ultrasonography identified a mass in the right testis. These findings were consistent with a testicular germ cell tumor, and the patient was promptly referred to oncology for further management.
References
The Illustration was created in https://BioRender.com
Braunstein, G. D. 1999. „Aromatase and Gynecomastia“. Endocrine-Related Cancer 6 (2): 315–24. https://doi.org/10.1677/erc.0.0060315.
Braunstein, Glenn D. 2007. „Clinical Practice. Gynecomastia“. The New England Journal of Medicine 357 (12): 1229–37. https://doi.org/10.1056/NEJMcp070677.
Chan, W. B., V. T. Yeung, C. C. Chow, W. Y. So, und C. S. Cockram. 1999. „Gynaecomastia as a Presenting Feature of Thyrotoxicosis“. Postgraduate Medical Journal 75 (882): 229–31. https://doi.org/10.1136/pgmj.75.882.229.
Chopra, I. J. 1975. „Gonadal Steroids and Gonadotropins in Hyperthyroidism“. The Medical Clinics of North America 59 (5): 1109–21. https://doi.org/10.1016/s0025-7125(16)31961-7.
Gordon, D. L., J. L. Brown, N. V. Emanuele, und L. Hall. 1997. „Gynecomastia as the Initial Manifestation of Hyperthyroidism“. Endocrine Practice: Official Journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists 3 (2): 80–81. https://doi.org/10.4158/EP.3.2.80.
Ho, H. K., und K. C. Loh. 1998. „Hyperthyroidism with Gynaecomastia as the Initial Complaint: A Case Report“. Annals of the Academy of Medicine, Singapore 27 (4): 594–96.
© 2025 EndoCases. All rights reserved.
This platform is intended for medical professionals, particularly endocrinology residents, and is provided for educational purposes only. It supports learning and clinical reasoning but is not a substitute for professional medical advice or patient care. The information is general in nature and should be applied with appropriate clinical judgment and in accordance with local guidelines.
Portions of the text on this website were edited with the assistance of Artificial Intelligence to improve grammar and phrasing, as English is not my first language. All medical content, ideas for illustrations, and overall structure are original and based on the author’s own expertise and the cited medical literature. No AI tools were used to generate or influence the educational content itself.
All of the content is independent of my employer.
Use of this site implies acceptance of our Terms of Use
Contact us via E-Mail: contact@endo-cases.com