The Framework
A Systematic Approach to Every Endocrine Patient—Structured, Reliable, and Complete.
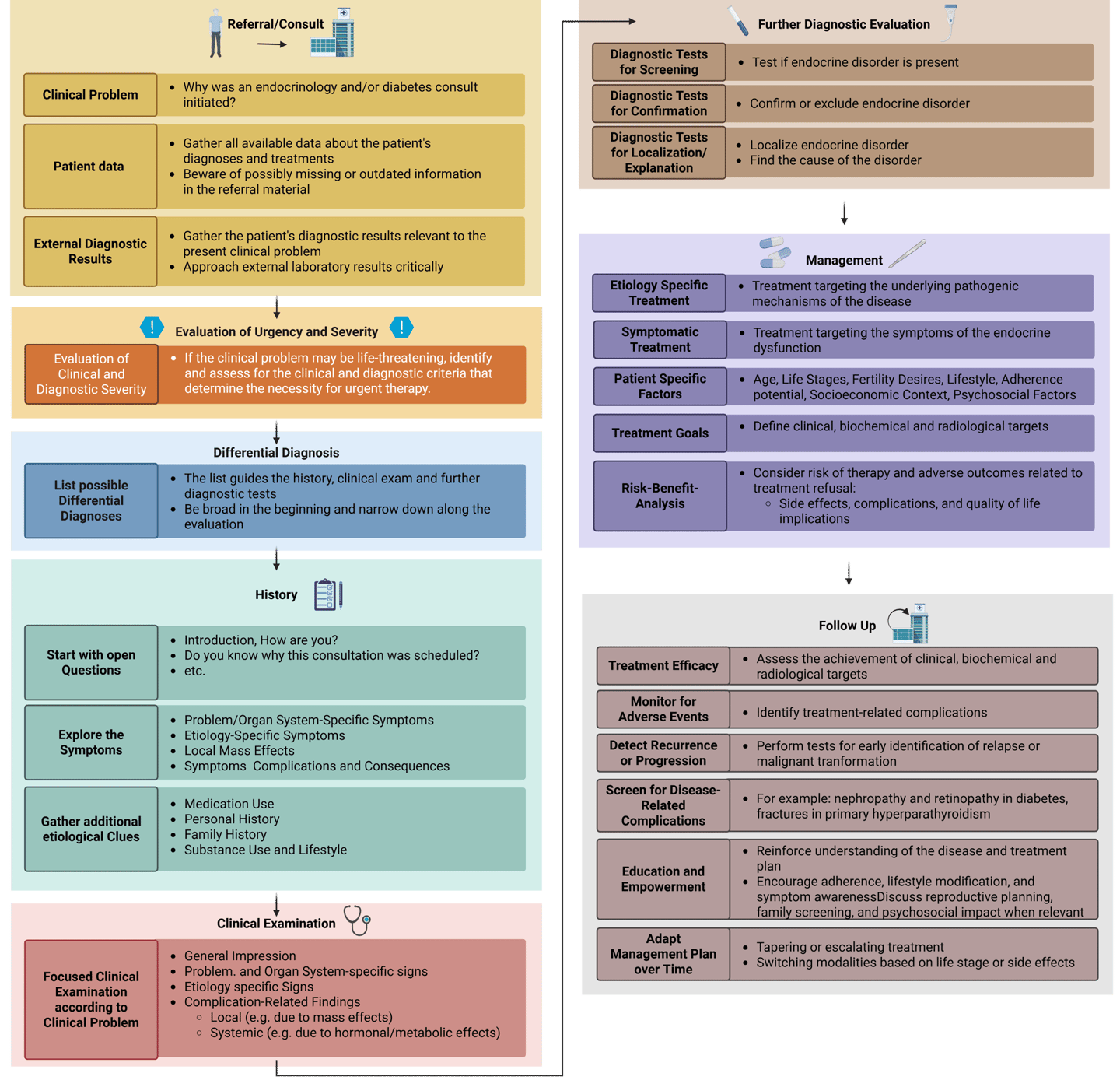
In clinical endocrinology, every patient presents a unique puzzle, but a systematic framework can guide your reasoning and decision-making. This framework provides a structured approach to any endocrine problem, helping you:
Think systematically so you don’t overlook critical information
Organize your assessment from history and examination to diagnostics and management
Apply a consistent method across different conditions, making complex cases more approachable
Build confidence in clinical reasoning and decision-making
This approach is particularly valuable when you are seeing a patient for the first time, where limited information is available at the start. The framework is deliberately structured this way for didactic purposes—to support systematic learning and reasoning. In real clinical practice, management may differ due to organizational workflows, available information, or institutional protocols, but the underlying logic of the framework remains a reliable guide.
By following this framework, you’ll have a practical tool that turns uncertainty into structured thinking and ensures no key step is missed—whether you’re tackling common endocrine problems or complex cases.
Created in https://BioRender.com Biedermann, R. (2025)
Clinical Framework for Clinical Practice in Endocrinology: Problem Solving with a structured approach
Just as in any other medical specialty, endocrinology greatly benefits from a structured approach to clinical problem solving. The classical evaluation of an endocrine issue typically follows a series of key steps in this order:
Referral/Consult request
Comprehensive history taking
Focused physical examination
Relevant diagnostic testing
Initial management planning
Follow-up care
As outlined below, I recommend explicitly incorporating two additional steps when evaluating a patient with a suspected endocrine disorder: an early assessment of the potential risk for life-threatening conditions and an early formulation of possible differential diagnoses. These steps help to structure the patient encounter and guide further evaluation. Therefore, I propose the following steps for patient evaluation:
Referral
Evaluation of Urgency and Severity
List Differential diagnoses
Comprehensive history taking
Focused physical examination
Relevant diagnostic testing
Initial management planning
Follow-up care
Based on these steps, I propose a framework that outlines the essential components of endocrinology practice that can be applied as a foundation for the approach to any clinical problem in endocrinology. While the specific structure may vary depending on individual preferences or clinical context, the core principle remains the same: a systematic approach is essential. In my experience, following such a method improves diagnostic accuracy, prevents premature or incorrect conclusions, and ensures that no important aspects of patient care are missed.
The clinical cases in this learning resource are organized according to this structured approach. You are encouraged to use the framework as presented, adapt it to suit your needs, and ultimately develop a consistent, intentional method for solving clinical problems—one that supports both your learning and your practice.
Framework of the Clinical Consultation in Endocrinology
A more detailed exploration of each component is provided further below.
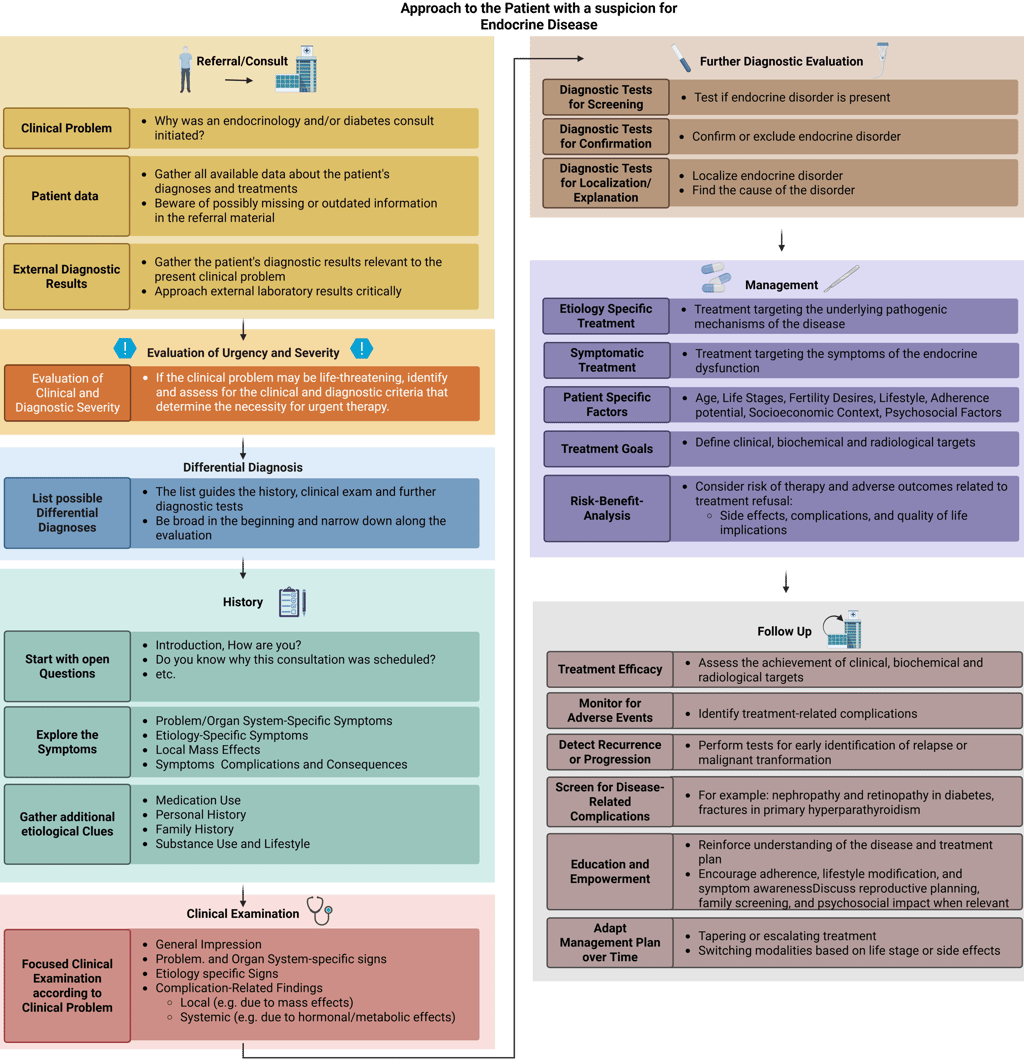
Created in https://BioRender.com Biedermann, R. (2025)
1. Referral/Consult
Referrals are a fundamental part of endocrine practice—they enable the endocrinologist to do their work and ensure that patients receive specialized care. Many referring physicians, especially experienced colleagues in primary care or other specialties, provide highly detailed and thoughtful referral information. These are invaluable and often reflect a strong understanding of endocrine problems. However, the quality and completeness of referral documentation can vary.
Referrals typically arrive as written letters summarizing the patient’s main complaint, initial diagnostic steps (such as lab results or imaging), and a list of current diagnoses and medications. In some settings, referrals may also occur via phone calls or electronic messages, especially when shared electronic medical records allow for direct chart review.
Despite their usefulness, referrals may have limitations. Common issues include:
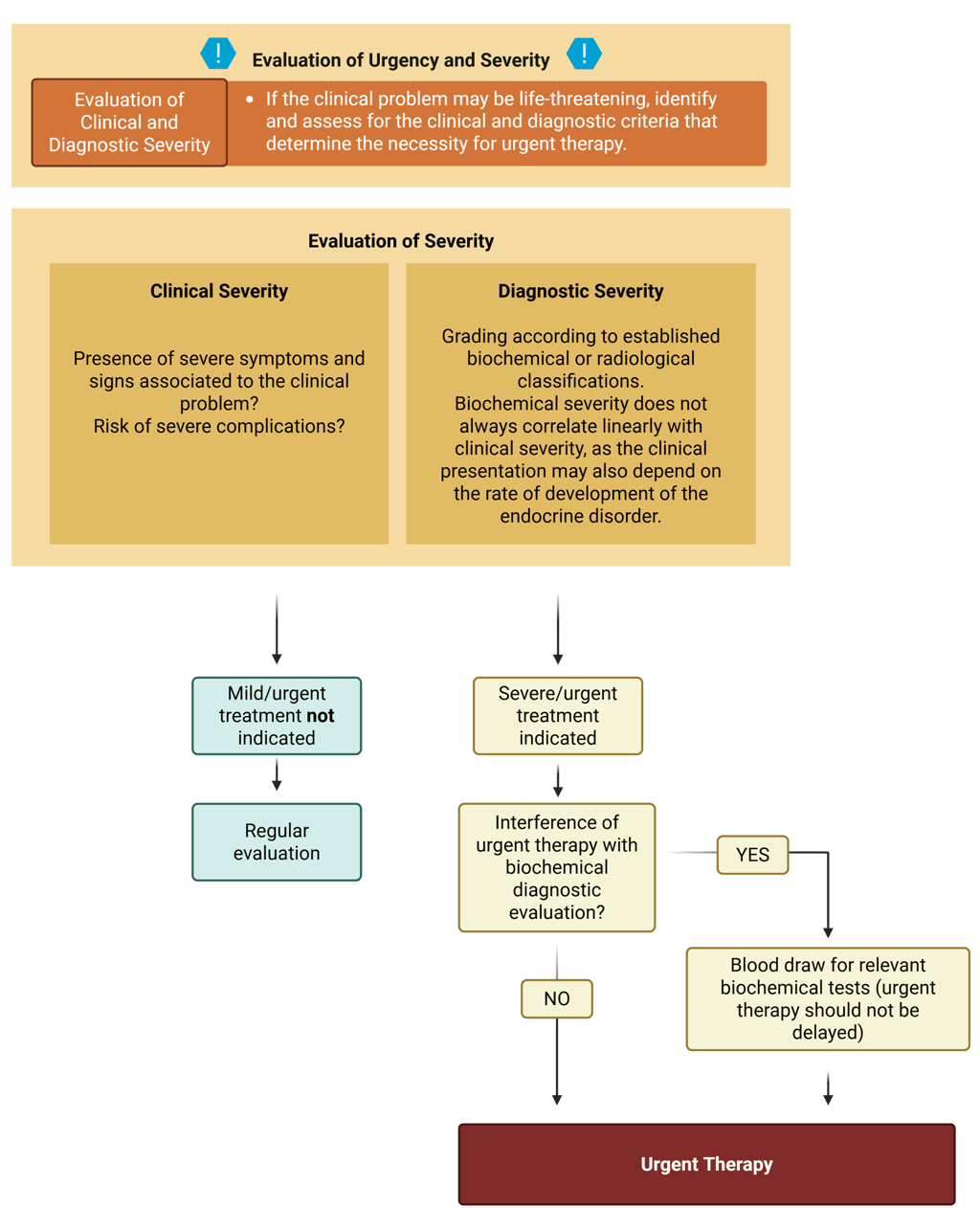
2. Evaluation of Urgency and Severity
Fortunately, the majority of clinical problems encountered in endocrinology and diabetes practice are not life-threatening. Nevertheless, important exceptions exist, including severe electrolyte disturbances (sodium, calcium, potassium, phosphate), thyroid storm, myxedema coma, adrenal insufficiency, diabetic ketoacidosis, etc. While such emergencies are relatively uncommon in routine outpatient care, they occur more frequently in the inpatient setting, where endocrinology and diabetes consultations include patients with acute or critical illnesses. In these situations, severe endocrine crises require prompt therapeutic intervention prior to detailed etiological evaluation (for example, a patient with severe symptomatic hyponatremia needs therapeutic interventions to prevent further complications before knowing the exact cause of the hyponatremia). It is therefore essential to be familiar with the criteria that guide the assessment of severity and the initiation of urgent therapy. These criteria usually include the presence of symptoms and signs that are classified as severe (clinical severity) and the biochemical grade of severity.
Depending on the situation, clinical severity may be evaluated either by yourself or by instructing the primary care providers to do so. Moreover, because therapeutic measures may interfere with diagnostic accuracy, blood samples for laboratory evaluation should be obtained before treatment is initiated whenever possible, without delaying the urgent treatment.
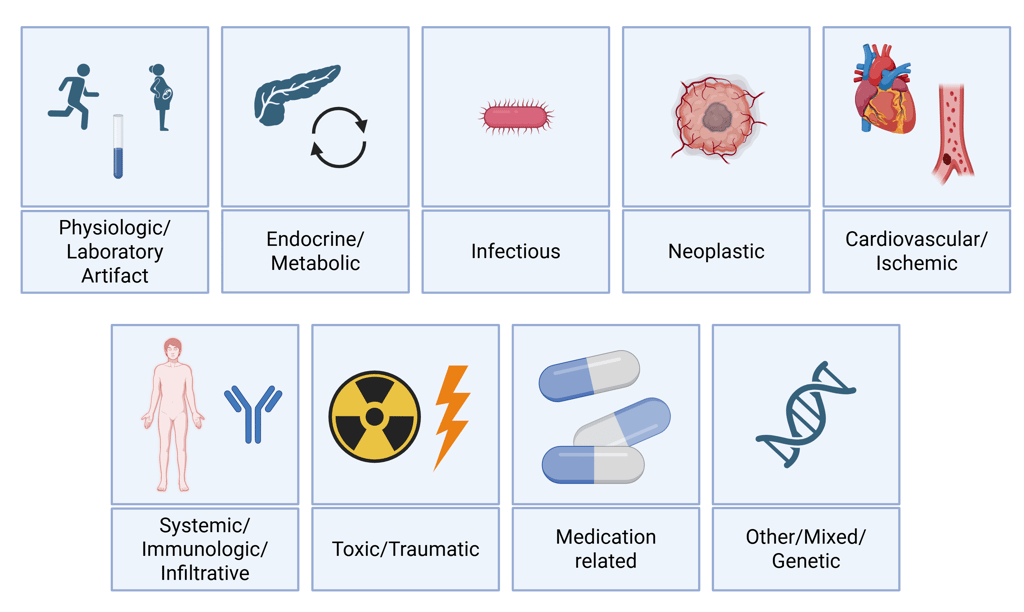
3. List possible Differential Diagnoses
When confronted with an endocrine clinical problem, formulating a differential diagnosis early is highly beneficial, as it guides both the focused history-taking and the communication with the requesting consultant. While comprehensive lists of differential diagnoses can always be reviewed later, it is essential to know the most important and common etiologies by heart. This not only improves efficiency but is particularly critical in situations where consultations are requested by phone, requiring the clinician to have the key diagnostic considerations and questions readily available. In my opinion, a structured approach to listing differential diagnoses is key. I prefer to organize them into broad etiological categories, which helps ensure that my initial considerations are comprehensive and that no important possibility is overlooked.
4. History Taking: The First Encounter with the Patient and Most Critical Step
A comprehensive and structured history forms the cornerstone of every clinical encounter, particularly in endocrinology. Many endocrine disorders have subtle presentations, evolve gradually, or mimic other conditions, making a systematic approach essential for accurate diagnosis, narrowing differential diagnoses, and guiding appropriate investigations and treatment.
Traditionally, the medical history is organized into the following domains:
History taking is not merely about collecting information; it involves generating hypotheses, identifying red flags, and understanding the broader context of the patient’s condition. It informs every subsequent step—from the physical examination to laboratory and imaging investigations, and ultimately to management decisions.
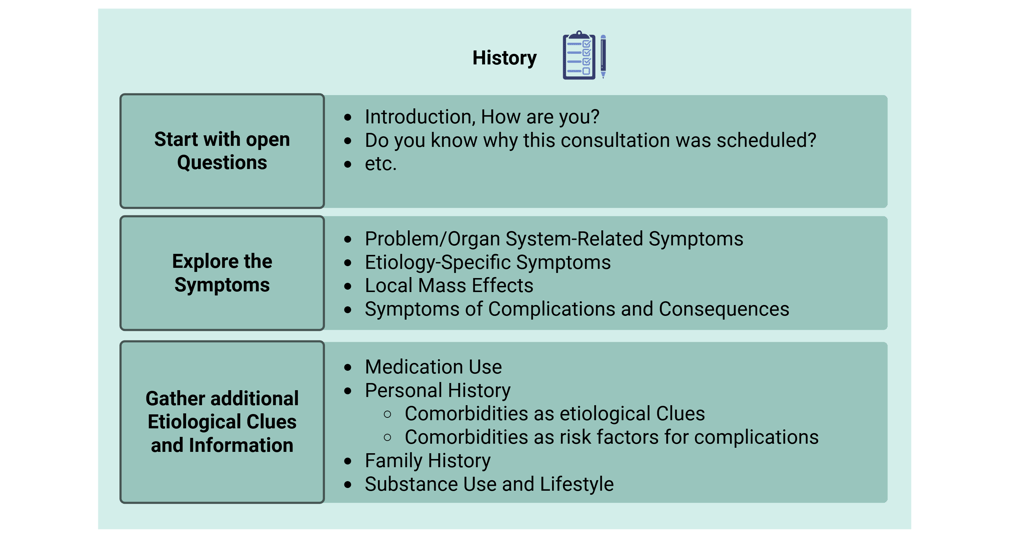
To maximize effectiveness, we recommend structuring endocrine history taking as follows:
The following sections elaborate on these key pillars of an effective endocrine history, integrating clinical reasoning and essential background knowledge to enable meaningful exploration and optimal diagnostic evaluation.
Start with an introduction and open questions
Starting with an introduction may seem self-explanatory, but it's an important step in building rapport and setting a professional tone. I recommend clearly stating your name and role, and briefly explaining the focus of your medical specialty. For example:
“Nice to meet you. My name is [...], I’m an endocrinologist and diabetologist. That means I evaluate and treat conditions related to hormone balance and sugar metabolism.”
This approach helps the patient understand who you are, what your role is, and what to expect from the consultation—especially important in complex specialties like endocrinology.
Open Questions, such as “How are you?” or “Do you know why you’re here today?” serve as effective openers in a medical consultation for several reasons:
They allow the patient to describe their clinical concerns in their own words, providing an early opportunity to express their thoughts, worries, and expectations.
They offer insight into how well the patient understands the reason for their endocrine or diabetes referral, and may also reveal their personal preferences or concerns regarding further evaluation or treatment.
Problem-/Organ Related Symptoms
Ask about associated symptoms related to the suspected endocrine system (e.g. in suspected thyroid disease, asking about energy levels, temperature sensitivity, bowel habits, hair loss, and changes in weight, mood, or menstrual cycle).
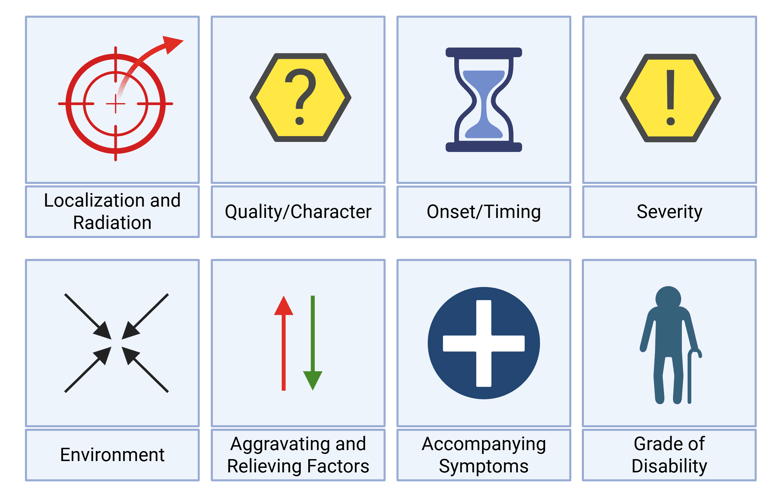
Explore all dimensions of the reported symptoms (Localization and radiation, quality, onset and duration, severity, triggers and relievers, accompanying symptoms, and grade of disability), similar to that of Kroenke, Kurt. 2014. „A Practical and Evidence-Based Approach to Common Symptoms: A Narrative Review“. Annals of Internal Medicine 161 (8): 579–86.https://doi.org/10.7326/M14-0461.

Ask about Condition-Specific Symptoms
Certain symptoms are specific to particular endocrine etiologies; for example, endocrine orbitopathy is characteristic of Graves disease as a cause of thyrotoxicosis. Eliciting these distinctive features can provide valuable clues to the underlying etiology.
Local Mass Effects
Asking specifically about symptoms caused by anatomical enlargement or tumor growth of endocrine organs.
Complications and Consequences
Ask about the secondary effects of long-standing or severe hormonal disturbances (e.g. osteoporotic fractures in hyperparathyroidism or postmenopausal hypogonadism).
Etiological Clues and Additional Information
Medication use
Always inquire about prescription drugs, over-the-counter medications, supplements, and vitamins
Personal Medical History
Gather Etiological Clues: Ask for or check the medical record for comorbidities associated with endocrine diseases
Gather more Information:
Childhood/adolescent development: may indicate new vs. long-standing endocrine disease
Risk factors for complications in association with endocrine disease (e.g. worsening of cardiac failure in thyrotoxicosis)
Family History
Ask about endocrine disorders, tumors or autoimmune diseases
Substance Use (Alcohol, Nicotine, Drugs) and Lifestyle
Assess for lifestyle factors that may affect endocrine function
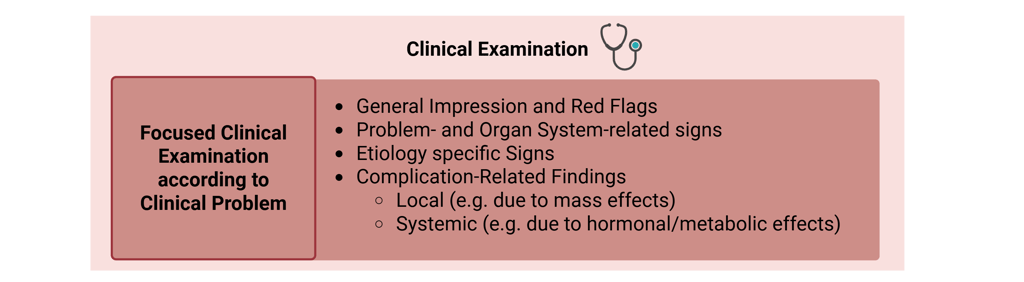
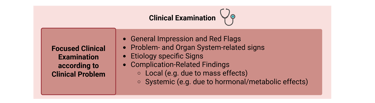
5. Clinical Examination
The physical exam remains indispensable. It can bring clinical context to reported symptoms or measured laboratory values. The goal is to identify and localize pathology, to corroborate or challenge the initial working diagnosis, and to detect systemic or organ-specific complications. Since endocrine diseases, if untreated, often progress over time, usually the clinical picture also becomes more evident over time. Below are the main components of an effective clinical examination in endocrinology:
General Impression and Red Flags: vital signs, general appearance, habitus, etc.
Problem-/Organ-Related signs: Examination of the suspected pathological endocrine organ or system. Integrating both local findings and systemic signs of the suspected disorder, e.g. goiter and signs of thyroid dysfunction, testes and gynecomastia, hair growth, etc.
Condition-Specific Signs: Certain signs are characteristic of specific underlying conditions. Recognizing and actively assessing these signs can provide a significant diagnostic advantage.
Complication-related findings:
Local: e.g. due to mass effects (visual field testing in suspected pituitary pathology, etc.)
Systemic: e.g. due to metabolic effects (neuropathy in diabetes mellitus, etc.)
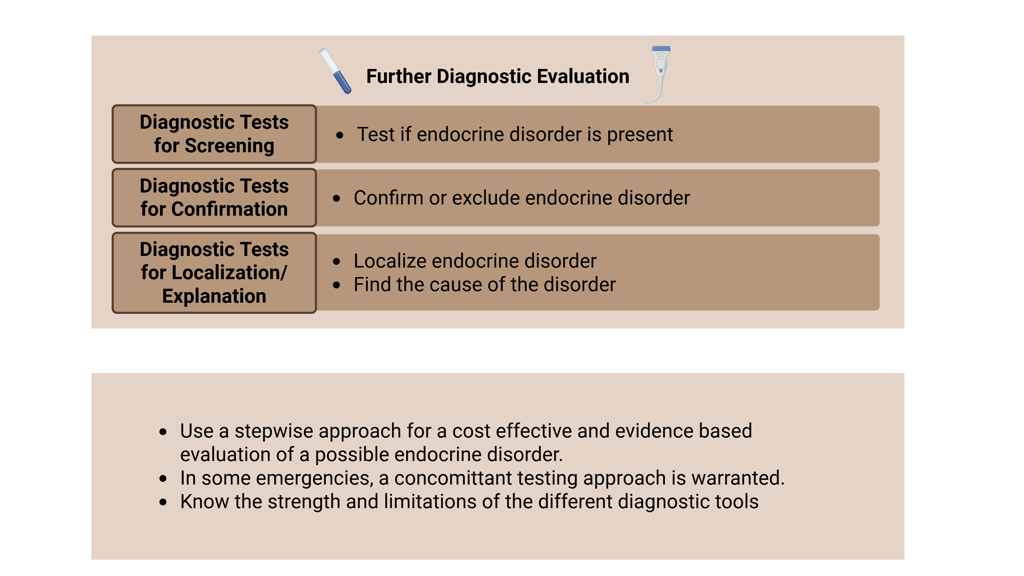
6. Diagnostic Approach: From Differential Diagnosis to Targeted Testing
Endocrine Diagnoses are made by combining the symptoms and clinical signs to a compatible diagnostic result (e.g. Laboratory, Radiology etc.). If the clinical picture does not match with an endocrine disorder, clinicians should refrain from ordering diagnostic tests, since this leads to unnecessary confusion and burden for the patient.
While the initial list of differential diagnoses already shaped how we asked questions and performed the clinical exam, this is the point to explicitly revisit and refine this list. Before jumping into tests, take a step back: based on history and exam, what are the most likely diagnoses, and what are the key alternatives that must not be missed?
Once the working diagnoses, based on the refined list differentials, are established, the diagnostic process should follow a logical and stepwise path. In most endocrine disorders, the approach aims to answer three core questions in sequence:
Initial Test or Screening Test: Could an endocrine disorder be present?
Example: Basal Cortisol testing for suspected adrenal insufficiency
Confirmatory Testing: can we confirm its presence?
Example: ACTH stimulation test to confirm adrenal insufficiency
Localization Tests and further diagnostic tests: What is the Cause?
Example: ACTH and Renin measurements, Pituitary MRI or adrenal imaging depending on suspected localization of adrenal insufficiency. Additional tests to evaluate etiologies (autoimmune disease, granulomatous diseases etc).
In certain clinical situations, such as emergencies, rapid diagnostic evaluation with concomitant testing is warranted.
The selection and sequence of diagnostic tests are grounded in endocrine physiology and pathophysiology. A thorough understanding of these principles allows for appropriate test ordering to screen, confirm, and differentiate among potential diagnoses. Rather than relying solely on flowcharts or predefined lists of tests, I strongly encourage approaching diagnostic evaluation from a pathophysiological perspective.
When interpreting results, it is important to integrate factors such as the strengths and limitations of the tests, the conditions under which they were performed, and the underlying endocrine physiology and pathophysiology.
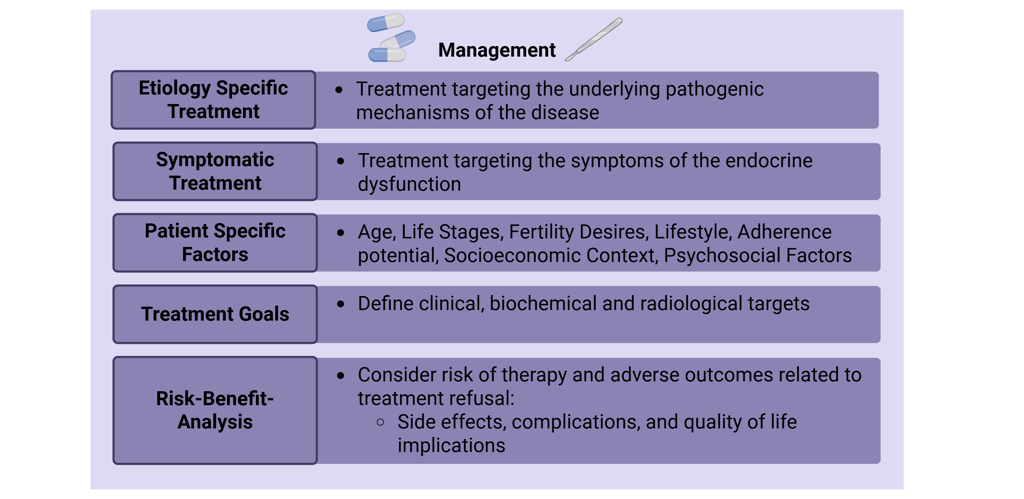
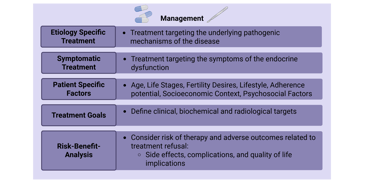
7. Management From Diagnosis to Treatment
Once a diagnosis is confirmed, the next step is to outline the therapeutic options to the patient. A thoughtful therapeutic plan balances disease-specific recommendations with patient-centered decision-making.
Knowledge of what treatments exist is the foundation, but it’s also important to understand when and for whom each option is appropriate. It’s a process that involves patient education, shared decision-making, and aligning medical possibilities with patient goals. The following are the core considerations for outlining treatment options.
Pathogenic Mechanism of Disease
Whenever possible, management should target the underlying cause and pathophysiological mechanism of the disorder—for example, surgical resection of a cortisol-producing pituitary adenoma in Cushing’s disease or pharmacologic interventions aimed at the specific pathogenic pathway in cases of hypercalcemia.
If this is not possible, or in emergency situations, a symptoms-oriented therapeutic approach should be adopted?
Patient-Specific Factors: Not all treatments are appropriate for every patient. A personalized approach considers:
Age and life stage (e.g., young adults vs. geriatric patients)
Comorbidities (e.g., heart disease, renal failure, cancer history)
Fertility desires and reproductive planning
Lifestyle, adherence potential, socioeconomic context (considering access to medications, ability to follow treatment plans, and financial aspects)
Psychosocial factors (e.g., mental health, support systems, cultural considerations)
Treatment Goals: Define therapeutic success and outline realistic expectations before initiating treatment.
What are the clinical, biochemical and radiological targets? What can and cannot be expected of the treatment?
Risk-Benefit Analysis: Assess short- and long-term risks of available interventions and compare them to potential benefits.
For Example: Medical vs. surgical options (e.g. medical management of an aldosterone producing adenoma vs. surgical therapy)
Side effects, complications, and quality of life implications
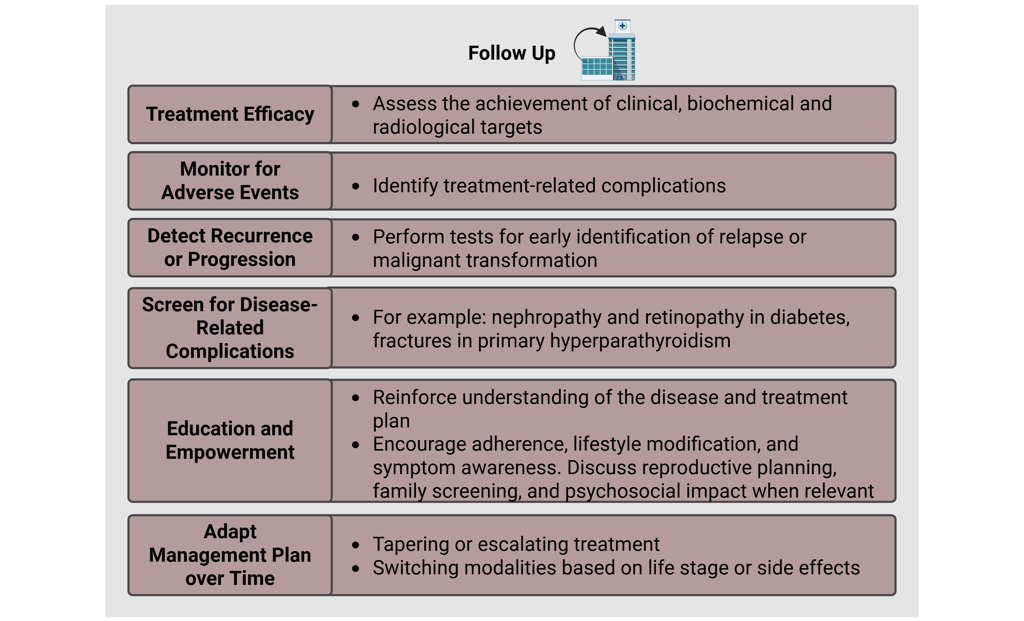
8. Follow-Up and Long-Term Management
Once treatment is established, the main goals of follow-up are to assess whether therapeutic targets are being met, detect side effects or complications early, monitor for disease recurrence or progression, and support the patient in managing their condition over time.
Many endocrine disorders require long-term or even lifelong care, making structured follow-up a critical component of high-quality endocrinology practice. It is during follow-up that treatment plans are fine-tuned, patient education becomes central, and outcomes are continuously evaluated and improved.
Assess Therapeutic Efficacy
Clinically: Is the patient feeling better or worse? Have symptoms improved?
Biochemically: Are biochemical targets being reached?
Radiologically (if applicable): what are the post-therapeutic imaging results?
Monitor for Adverse Effects
Identify treatment-related complications (e.g. valvulopathy in dopamine agonist use)
Detect Recurrence or Progression
Some disorders require surveillance for relapse or malignant transformation (e.g. thyroid cancer, adrenal incidentalomas)
Screen for Disease-Related Complications
For example: nephropathy and retinopathy in diabetes, fractures in primary hyperparathyroidism
Educate and Empower the Patient
Reinforce understanding of the disease and treatment plan
Encourage adherence, lifestyle modification, and symptom awareness
Discuss reproductive planning, family screening, and psychosocial impact when relevant
Adapt the Plan Over Time
Tapering or escalating treatment
Switching modalities based on life stage or side effects
References
All Illustrations on this page were created in https://BioRender.com
Kroenke, Kurt. 2014. „A Practical and Evidence-Based Approach to Common Symptoms: A Narrative Review“. Annals of Internal Medicine 161 (8): 579–86.https://doi.org/10.7326/M14-0461.
Frequently Asked Questions
What is this platform about?
This platform provides clinical cases for endocrinology residents to enhance their learning experience.
Who can use this platform?
Endocrinology residents and medical students can utilize this platform for educational purposes and clinical case studies.
How are cases structured?
Clinical cases are organized systematically to facilitate a structured learning approach for residents in endocrinology.
Is there a privacy policy?
Yes, we have a privacy policy to protect user data and ensure confidentiality.
How can I contact support?
You can reach our support team via the contact form on our website.
Are there any fees involved?
Access to the platform is free for all registered users, ensuring equitable learning opportunities.
© 2025 EndoCases. All rights reserved.
This platform is intended for medical professionals, particularly endocrinology residents, and is provided for educational purposes only. It supports learning and clinical reasoning but is not a substitute for professional medical advice or patient care. The information is general in nature and should be applied with appropriate clinical judgment and in accordance with local guidelines.
Portions of the text on this website were edited with the assistance of Artificial Intelligence to improve grammar and phrasing, as English is not my first language. All medical content, ideas for illustrations, and overall structure are original and based on the author’s own expertise and the cited medical literature. No AI tools were used to generate or influence the educational content itself.
All of the content is independent of my employer.
Use of this site implies acceptance of our Terms of Use
Contact us via E-Mail: contact@endo-cases.com





