How I Approach the Patient with Hyponatremia
Hyponatremia is a notoriously tough clinical problem for residents.
While many different flowcharts exist for approaching it, they can be hard to recall unless you understand the reasoning behind each step. Personally, I find it more effective to think of the diagnostic process as a structured sequence of questions, each paired with the relevant tests that guide decision-making:
Is urgent treatment indicated?
Are moderate or severe symptoms present?
Is hyponatremia acute?
What is the tonicity?
Hypotonic, isotonic, or hypertonic?
Is the hyponatremia AVP-dependent?
Is the urine osmolality above or below 100 mOsm/kg?
Is AVP secretion appropriate?
How high is urine sodium (UNa)?
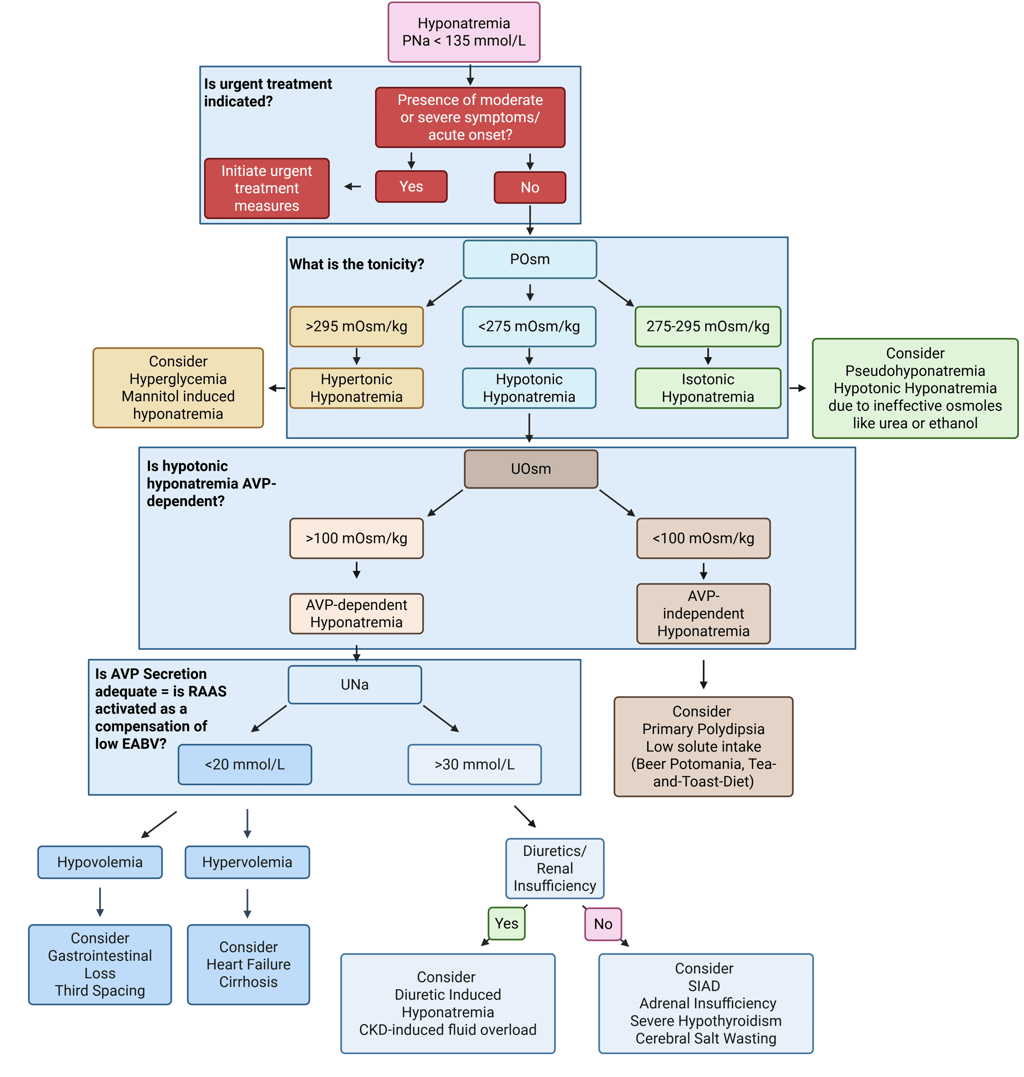
Illustration: Diagnostic Flowchart of hyponatremia, adapted from Workenehet al. 2023. „Hyponatremia Demystified: Integrating Physiology to Shape Clinical Practice“. Advances in Kidney Disease and Health 30 (2): 85–101. https://doi.org/10.1053/j.akdh.2022.11.004.
Is urgent treatment indicated?
Because of its clinical variability and potential for emergency, hyponatremia should always be considered early and managed promptly. This is done by assessing the rate of onset, the clinical presentation and biochemical severity.
What is the tonicity?
The first step in evaluating hyponatremia is to determine whether it is associated with hypotonicity (and therefore is "true hyponatremia". This is assessed by measuring serum osmolality (SOsm). A low SOsm (<275 mOsm/kg) confirms hypotonic hyponatremia.
Is the hyponatremia AVP-dependent?
In the case of Hypotonic Hyponatremia, the next step is to determine whether the hypotonic hyponatremia is mediated by arginine vasopressin (AVP). This can be assessed by evaluating urine osmolality (UOsm). If the urine is not maximally dilute (UOsm > 100 mOsm/kg), it suggests that AVP is active and contributes to water retention. Conversely, a maximally dilute urine (UOsm < 100 mOsm/kg) indicates AVP-independent hypotonic hyponatremia.
Is AVP secretion appropriate?
If hypotonic Hyponatremia is AVP dependent, the next step is to assess whether AVP secretion is appropriate in the context of hypotonic hyponatremia. Among the possible triggers, a reduction in effective arterial blood volume (EABV) is the only physiologically valid stimulus for AVP release under these conditions.
When EABV is decreased, as seen in hypovolemia, heart failure, or cirrhosis, the body activates the renin-angiotensin-aldosterone system (RAAS), which promotes sodium retention. In such cases, urinary sodium concentration (UNa) is typically low, often less than 20 mmol/L.
On the other hand, a UNa greater than 30 mmol/L generally suggests that RAAS is not fully activated, implying that EABV is normal, elevated, or at least does not play the main role in hyponatremia pathogenesis. In this setting, ongoing AVP secretion is not appropriate
You may observe that this flowchart (as well as the one in the original article) does not include volume status as part of the diagnostic approach to hyponatremia. I personally prefer the physiology-based strategy for diagnosing hyponatremia proposed by Workeneh et al rather than the traditional volume status–based algorithm, because clinical evaluation of extracellular fluid (ECF) volume often lacks sensitivity and specificity in this context, as already mentioned above. Nonetheless, I still recommend conducting a clinical assessment of volume status, ideally supported by point-of-care ultrasound, to help identify signs of cardiac decompensation, especially since this assessment is typically done before laboratory results are available.
Whether you use this exact flowchart or another, maintaining a systematic approach to hyponatremia not only clarifies the diagnostic process but also ensures accurate identification of the underlying cause and timely initiation of appropriate therapy. True diagnostic clarity comes from understanding the pathophysiological reasoning behind every test.
References
All Illustrations were created in https://BioRender.com
Verbalis JG, Goldsmith SR, Greenberg A, Korzelius C, Schrier RW, Sterns RH, Thompson CJ. Diagnosis, evaluation, and treatment of hyponatremia: expert panel recommendations. Am J Med. 2013 Oct;126(10 Suppl 1):S1-42. doi: 10.1016/j.amjmed.2013.07.006. PMID: 24074529.
Goce Spasovski, Raymond Vanholder, Bruno Allolio, Djillali Annane, Steve Ball, Daniel Bichet, Guy Decaux, Wiebke Fenske, Ewout J. Hoorn, Carole Ichai, Michael Joannidis, Alain Soupart, Robert Zietse, Maria Haller, Sabine van der Veer, Wim Van Biesen, Evi Nagler, on behalf of the Hyponatraemia Guideline Development Group, Clinical practice guideline on diagnosis and treatment of hyponatraemia, Nephrology Dialysis Transplantation, Volume 29, Issue suppl_2, April 2014, Pages i1–i39, https://doi.org/10.1093/ndt/gfu040
Workenehet al. 2023. „Hyponatremia Demystified: Integrating Physiology to Shape Clinical Practice“. Advances in Kidney Disease and Health 30 (2): 85–101. https://doi.org/10.1053/j.akdh.2022.11.004.
© 2025 EndoCases. All rights reserved.
This platform is intended for medical professionals, particularly endocrinology residents, and is provided for educational purposes only. It supports learning and clinical reasoning but is not a substitute for professional medical advice or patient care. The information is general in nature and should be applied with appropriate clinical judgment and in accordance with local guidelines.
Portions of the text on this website were edited with the assistance of Artificial Intelligence to improve grammar and phrasing, as English is not my first language. All medical content, ideas for illustrations, and overall structure are original and based on the author’s own expertise and the cited medical literature. No AI tools were used to generate or influence the educational content itself.
All of the content is independent of my employer.
Use of this site implies acceptance of our Terms of Use
Contact us via E-Mail: contact@endo-cases.com