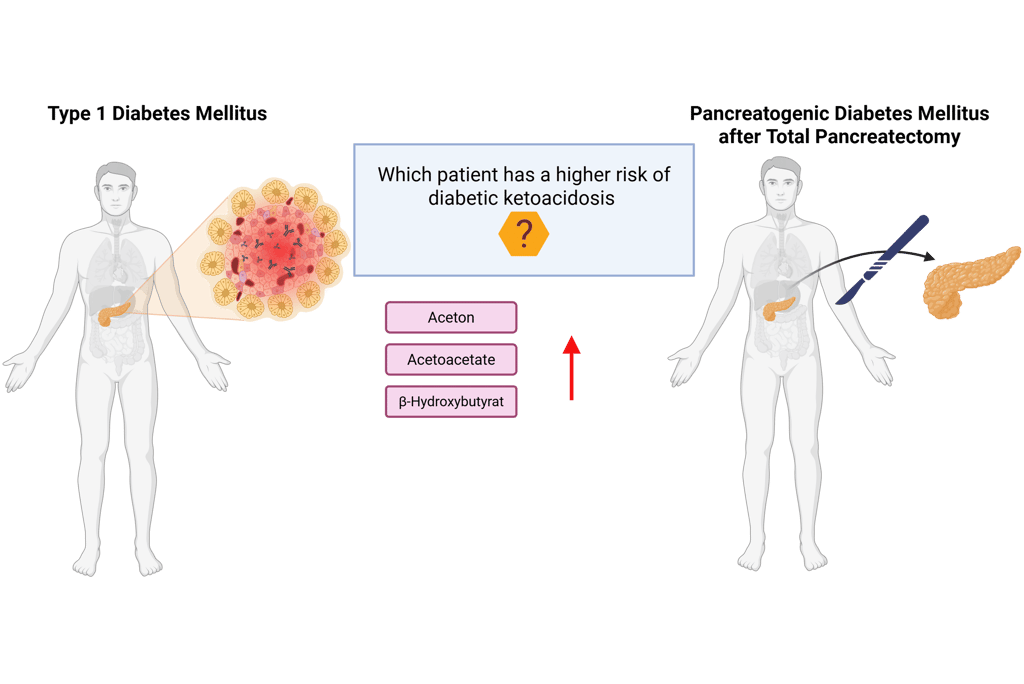
Diabetes Mellitus Type 1 vs Pancreatogenic Diabetes Mellitus after Total Pancreatectomy: Who is at higher risk for Diabetic Ketoacidosis?
Both type 1 diabetes mellitus (T1DM) and pancreatogenic diabetes mellitus (PDM) following total pancreatectomy are characterized by an absolute deficiency of endogenous insulin, making regular insulin administration essential to prevent hyperglycemia and diabetic ketoacidosis (DKA).
However, the risk of developing DKA in case of missed insulin doses differs between these two forms of insulin-deficient diabetes. Do you know who is at higher risk?
Patients with type 1 diabetes have a higher risk of DKA than those with pancreatogenic diabetes after total pancreatectomy. Do you know why?
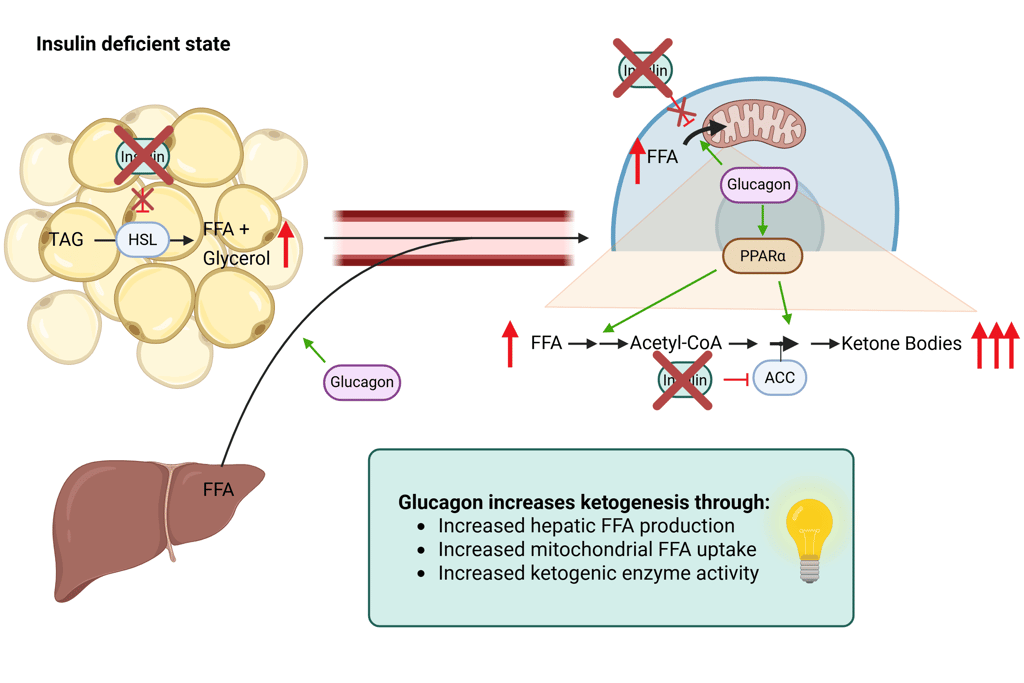
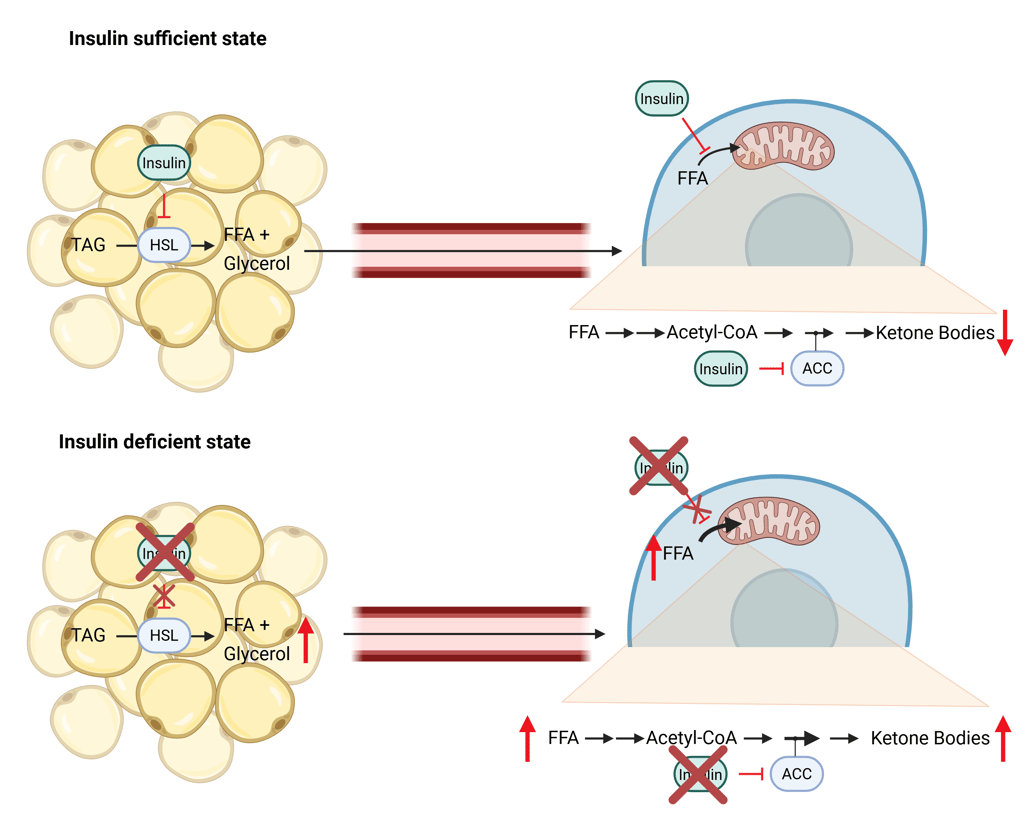
To understand why, it is helpful to recall how DKA develops. DKA results from an excessive accumulation of ketone bodies due to altered fatty acid metabolism in the setting of insulin deficiency. Insulin normally inhibits ketogenesis by regulating key enzymes in lipid metabolism. When insulin levels fall:
Free fatty acid (FFA) release increases — due to reduced inhibition of hormone-sensitive lipase (HSL).
FFA uptake into mitochondria increases — due to decreased activity of acetyl-CoA carboxylase (ACC), lowering malonyl-CoA and disinhibiting carnitine palmitoyltransferase 1 (CPT1).
Ketone body production increases — due to increased activity of HMG-CoA synthase.
Ketone bodies (acetoacetate, β-hydroxybutyrate, and acetone) are water-soluble organic acids. Their accumulation lowers blood pH, resulting in metabolic acidosis — the hallmark of DKA.
Ketogenesis is further stimulated by counterregulatory hormones such as glucagon, cortisol, catecholamines, and thyroid hormones, which enhance lipolysis and FFA availability.
Glucagon increases ketogenesis through:
Increased hepatic FFA production
Increased mitochondrial FFA uptake
Increased ketogenic enzyme activity
In pancreatogenic diabetes after total pancreatectomy, both insulin and glucagon secretion are absent. In contrast, in type 1 diabetes, only β-cells are targeted by the immune system, while α-cells (the source of glucagon) remain intact. Consequently, the strong glucagon-mediated drive for ketogenesis is preserved in type 1 diabetes, explaining the greater DKA risk compared to pancreatogenic diabetes after total pancreatectomy.
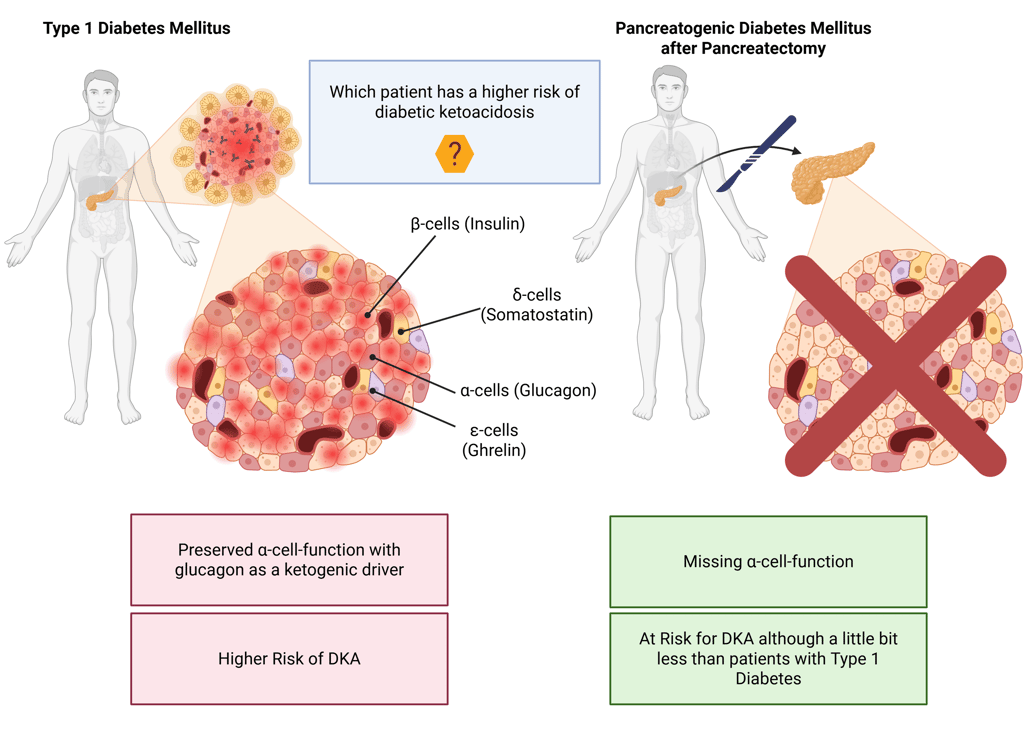
Note: Cell distribution in pancreas is illustrative and does not represent real histology accurately
References:
Dhatariya KK, Glaser NS, Codner E, Umpierrez GE. Diabetic ketoacidosis. Nat Rev Dis Primers. 2020 May 14;6(1):40. doi: 10.1038/s41572-020-0165-1. PMID: 32409703.
Veauthier B, Levy-Grau B. Diabetic Ketoacidosis: Evaluation and Treatment. Am Fam Physician. 2024 Nov;110(5):476-486. PMID: 39556629.
Palmer BF, Clegg DJ. Electrolyte and Acid-Base Disturbances in Patients with Diabetes Mellitus. N Engl J Med. 2015 Aug 6;373(6):548-59. doi: 10.1056/NEJMra1503102. Erratum in: N Engl J Med. 2019 Oct 17;381(16):1598. doi: 10.1056/NEJMx190026. PMID: 26244308.
All Illustrations were created in https://BioRender.com
© 2025 EndoCases. All rights reserved.
This platform is intended for medical professionals, particularly endocrinology residents, and is provided for educational purposes only. It supports learning and clinical reasoning but is not a substitute for professional medical advice or patient care. The information is general in nature and should be applied with appropriate clinical judgment and in accordance with local guidelines.
Portions of the text on this website were edited with the assistance of Artificial Intelligence to improve grammar and phrasing, as English is not my first language. All medical content, ideas for illustrations, and overall structure are original and based on the author’s own expertise and the cited medical literature. No AI tools were used to generate or influence the educational content itself.
All of the content is independent of my employer.
Use of this site implies acceptance of our Terms of Use
Contact us via E-Mail: contact@endo-cases.com