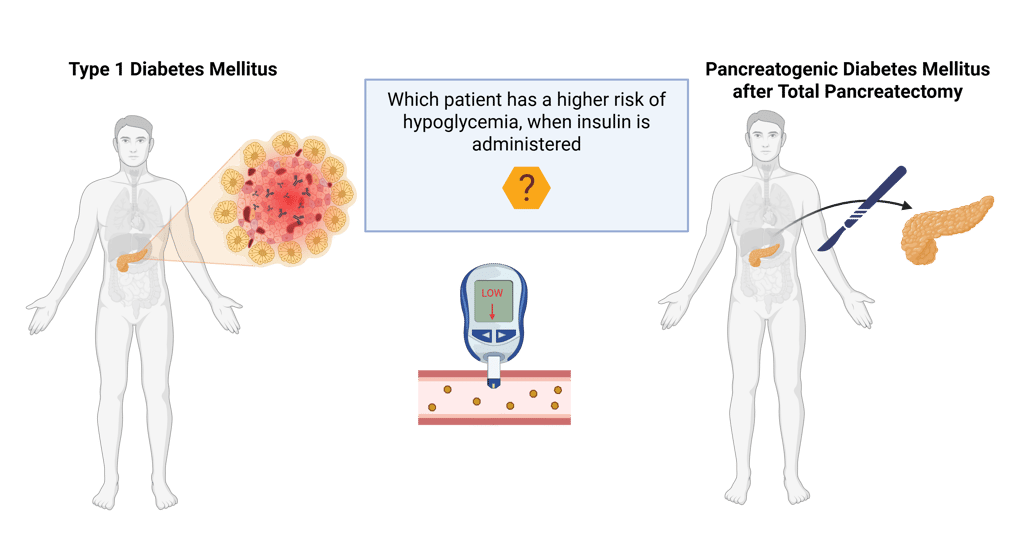
Diabetes Mellitus Type 1 vs Pancreatogenic Diabetes Mellitus after Total Pancreatectomy: Who is at higher risk for Hypoglycemia?
Insulin therapy is the mainstay of treatment for both type 1 diabetes mellitus (T1DM) and pancreatogenic diabetes mellitus (PDM) after total pancreatectomy. Because insulin lowers blood glucose, both groups of patients are at risk of developing hypoglycemia.
However, the risk of clinically significant hypoglycemia differs between these two forms of diabetes. Do you know, who is at higher risk for hypoglycemia?
Patients with pancreatogenic diabetes after total pancreatectomy are at higher risk.
To understand why, we need to recall how the body normally responds to falling blood glucose.
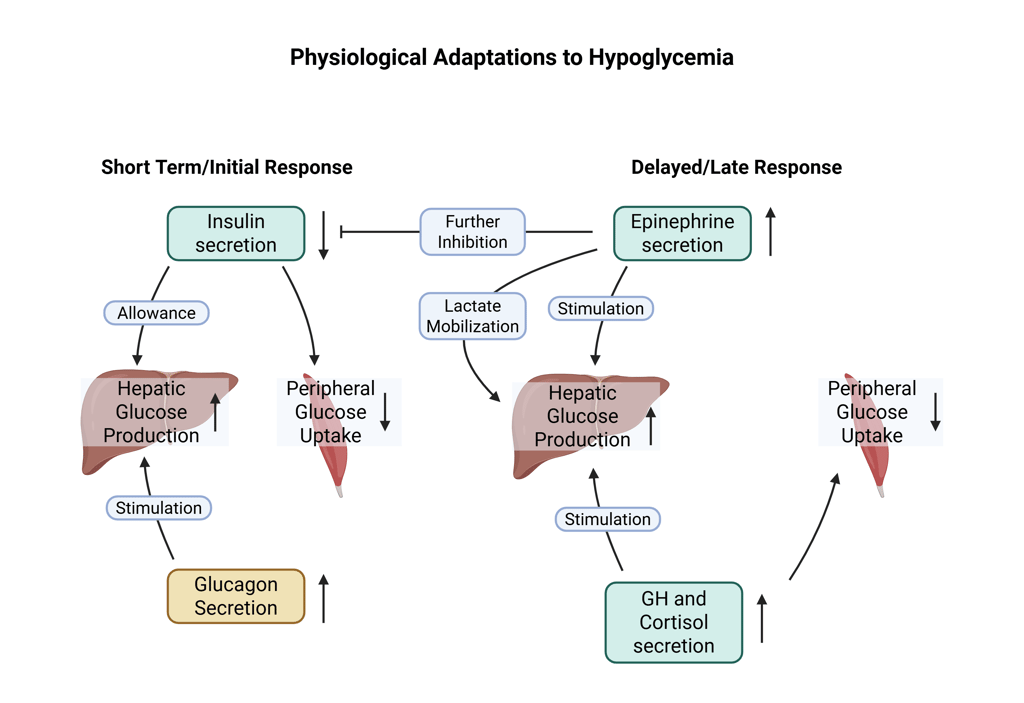
1. Immediate Response (within minutes)
The goal is to halt further glucose decline and restore hepatic glucose output.
Decreased Insulin secretion: Reduces peripheral glucose uptake, preserving circulating glucose. Lower insulin levels allow for an increase in hepatic glucose production (through gluconeogenesis and glycogenolysis).
Increased Glucagon secretion: Stimulates hepatic glycogenolysis and gluconeogenesis.
2. Delayed (Secondary) Response (minutes to hours)
These mechanisms sustain glucose production if hypoglycemia persists.
Increased Epinephrine (adrenaline) secretion: Enhances hepatic glucose production, inhibits insulin secretion, and mobilizes substrates für gluconeogenesis (e.g. lactate, amino acids).
Increased Cortisol and growth hormone secretion: Act over hours to support gluconeogenesis and reduce peripheral glucose utilization.
After total pancreatectomy, both β-cells and α-cells are absent.
This means patients lack not only insulin but also glucagon, the key immediate counterregulatory hormone.
In contrast, individuals with type 1 diabetes retain α-cell function and can still mount a glucagon response (at least early in the disease).
Furthermore, exogenous insulin continues to act even as glucose levels fall, because, unlike endogenous insulin, its secretion from the subcutaneous tissue cannot be physiologically reduced in response to hypoglycemia. This persistent insulin action prevents the body from counterbalancing falling glucose levels, amplifying the risk of severe or prolonged hypoglycemia.
Therefore, patients with pancreatogenic diabetes lack both mechanisms of the first line of defense against falling glucose, making them more prone to severe or prolonged hypoglycemia compared to patients with type 1 diabetes mellitus, and intact glucagon secretion.
Additional factors such as insulin sensitivity, dietary intake, alcohol consumption, and insulin dosing technique further modulate individual risk.
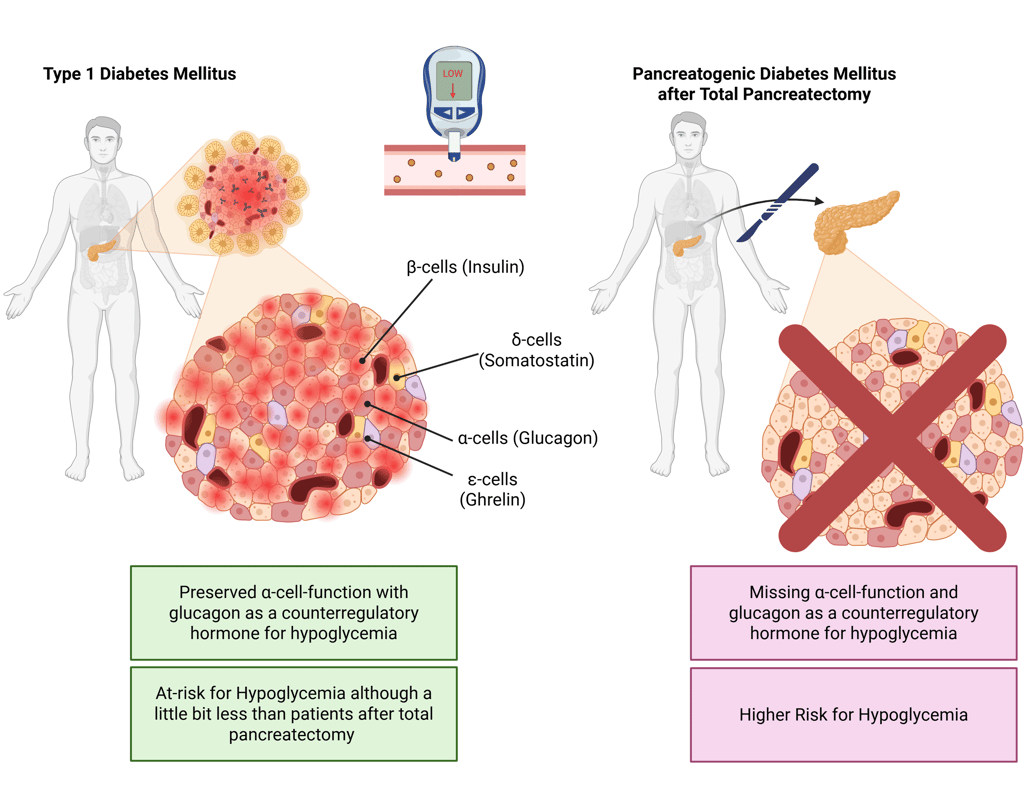
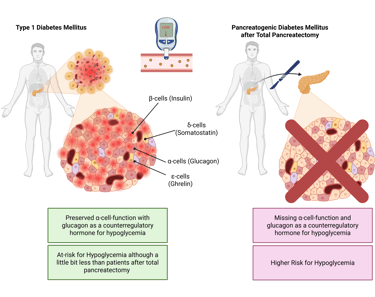
Note: Cell distribution in pancreas is illustrative and does not represent real histology accurately
References
All Illustrations are Created in https://BioRender.com
Hoffman RP. Sympathetic mechanisms of hypoglycemic counterregulation. Curr Diabetes Rev. 2007 Aug;3(3):185-93. doi: 10.2174/157339907781368995. PMID: 18220670.
Verhulst CEM, Fabricius TW, Teerenstra S, Kristensen PL, Tack CJ, McCrimmon RJ, Heller S, Evans ML, Amiel SA, Pedersen-Bjergaard U, de Galan BE; Hypo-RESOLVE consortium. Glycaemic thresholds for counterregulatory hormone and symptom responses to hypoglycaemia in people with and without type 1 diabetes: a systematic review. Diabetologia. 2022 Oct;65(10):1601-1612. doi: 10.1007/s00125-022-05749-8. Epub 2022 Jul 22. PMID: 35867127; PMCID: PMC9477942.
Davis MR, Shamoon H. Counterregulatory adaptation to recurrent hypoglycemia in normal humans. J Clin Endocrinol Metab. 1991 Nov;73(5):995-1001. doi: 10.1210/jcem-73-5-995. PMID: 1939537.
Stanley S, Moheet A, Seaquist ER. Central Mechanisms of Glucose Sensing and Counterregulation in Defense of Hypoglycemia. Endocr Rev. 2019 Jun 1;40(3):768-788. doi: 10.1210/er.2018-00226. PMID: 30689785; PMCID: PMC6505456.
© 2025 EndoCases. All rights reserved.
This platform is intended for medical professionals, particularly endocrinology residents, and is provided for educational purposes only. It supports learning and clinical reasoning but is not a substitute for professional medical advice or patient care. The information is general in nature and should be applied with appropriate clinical judgment and in accordance with local guidelines.
Portions of the text on this website were edited with the assistance of Artificial Intelligence to improve grammar and phrasing, as English is not my first language. All medical content, ideas for illustrations, and overall structure are original and based on the author’s own expertise and the cited medical literature. No AI tools were used to generate or influence the educational content itself.
All of the content is independent of my employer.
Use of this site implies acceptance of our Terms of Use
Contact us via E-Mail: contact@endo-cases.com