Preoperative Adrenergic Blockade in Pheochromocytoma: Why Sequence Matters
Pheochromocytoma is a catecholamine-producing neuroendocrine tumor arising from the chromaffin cells of the adrenal medulla. It synthesizes, stores, and secretes epinephrine and norepinephrine, leading to excessive adrenergic stimulation. Clinically, this most often presents with hypertension, headaches, palpitations, and diaphoresis, though the presentation can vary widely depending on the tumor’s secretory pattern and receptor sensitivity.
The definitive therapy is surgical removal (adrenalectomy). However, careful preoperative medical preparation is essential to prevent intraoperative hypertensive crises. This preparation includes sequential adrenergic blockade, beginning with α-adrenergic blockade, followed by the addition of β-blockade.
But do you know why adrenergic blockade must be initiated in this specific order?
To answer that, let’s briefly revisit the normal physiology of catecholamine effects.
Catecholamines exert their actions through G-protein coupled receptors, called adrenergic receptors, which are classified into α (α₁, α₂) and β (β₁, β₂, β₃) subtypes:
α₁-receptors are located on vascular smooth muscle and mediate vasoconstriction and increased blood pressure.
α₂-receptors function both presynaptically (inhibiting norepinephrine release) and postsynaptically, contributing to central and peripheral vascular control.
β₁-receptors in the heart increase heart rate and contractility.
β₂-receptors cause vasodilation and bronchodilation, while β₃-receptors in adipose tissue promote lipolysis and thermogenesis.
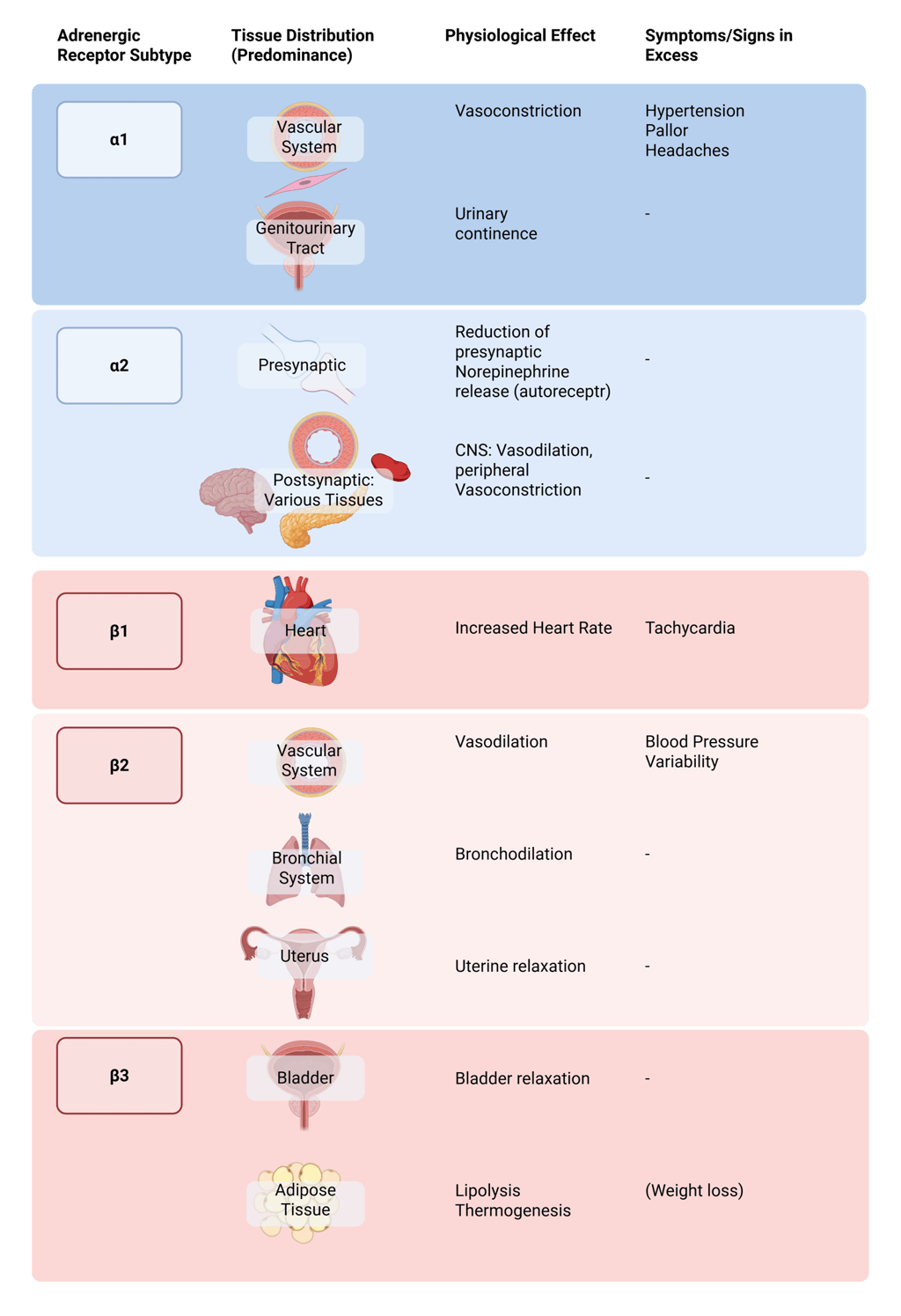
Illustration of adrenergic receptor subtypes, their effects upon activation and symptoms in excess. Sweating is another inportant symptom of catecholamine excess, not illustrated here. It is the result of the increased catecholaminesacting on α1- and β-adrenergic receptors in the skin and sweat glands, with both peripheral and central mechanisms contributing to increased diaphoresis.
Although both epinephrine and norepinephrine activate α- and β-receptors, they differ in their affinities:
Norepinephrine has a higher affinity for α₁-receptors, producing potent vasoconstriction and sustained elevations in blood pressure.
Epinephrine, which acts on both α and β receptors, predominantly stimulates β1 and β₂-receptors at low concentrations (causingincreased heart rate, vasodilation and bronchodilation), while at higher levels it shifts toward α₁-mediated vasoconstriction, leading to variable blood pressure effects.
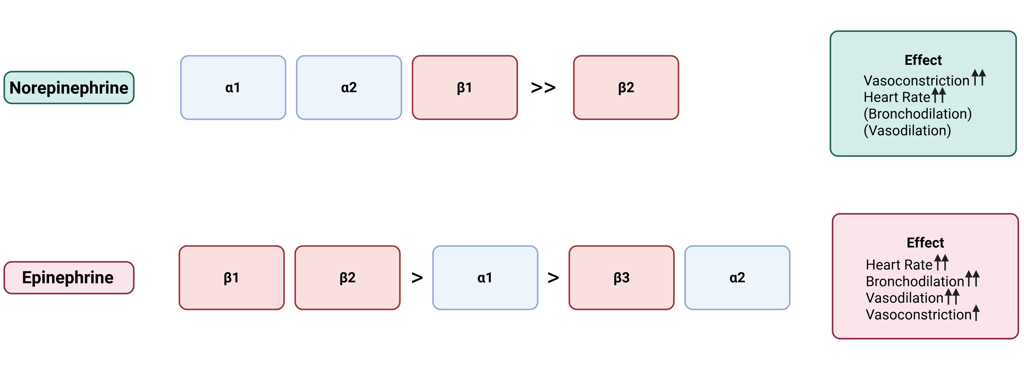
Illustration: Affinity of Norerpinephrine and Epinephrine on adrenergic receptor subtypes
Since most pheochromocytomas predominantly secrete norepinephrine, the result is sustained α-adrenergic vasoconstriction and hypertension.
Therefore, preoperative adrenergic blockade is initiated to prevent catecholamine-induced hypertensive crises during surgery. However, β-blockade before α-blockade is contraindicated, as it can precipitate a dangerous hypertensive crisis by leaving unopposed α-adrenergic stimulation.
This paradoxical rise in blood pressure occurs because circulating catecholamines, especially norepinephrine, continue to activate α-receptors, while β-receptors (including β₂-mediated vasodilatory pathways) are pharmacologically blocked.
Thus, α-adrenergic blockade is always initiated first (typically with phenoxybenzamine or doxazosin) to control hypertension and prevent catecholamine-induced vasoconstriction. β-blockade is added only after adequate α-blockade has been achieved to manage tachycardia or arrhythmias.
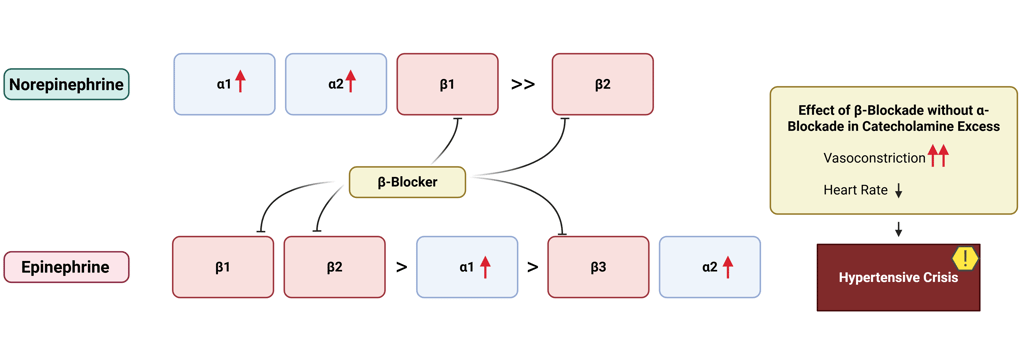
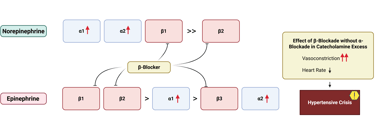
Illustration: unopposed α-adrenergic vasoconstriction in β-blockade therapy before α-blockade therapy in catecholamine excess
Important note:
Preoperative preparation for pheochromocytoma involves more than just adrenergic blockade and is typically performed under inpatient supervision. For detailed guidance, refer to the cited literature on perioperative management of pheochromocytomas.
References
All Illustrations were created in https://BioRender.com
E, Sbardella, und Grossman Ab. 2020. „Pheochromocytoma: An Approach to Diagnosis“. Best Practice & Research. Clinical Endocrinology & Metabolism 34 (2). https://doi.org/10.1016/j.beem.2019.101346.
H, Chen, Sippel Rs, O’Dorisio Ms, Vinik Ai, Lloyd Rv, und Pacak K. 2010. „The North American Neuroendocrine Tumor Society Consensus Guideline for the Diagnosis and Management of Neuroendocrine Tumors: Pheochromocytoma, Paraganglioma, and Medullary Thyroid Cancer“. Pancreas 39 (6). https://doi.org/10.1097/MPA.0b013e3181ebb4f0.
Ma, Nazari, Hasan R, Haigney M, u. a. 2023. „Catecholamine-Induced Hypertensive Crises: Current Insights and Management“. The Lancet. Diabetes & Endocrinology 11 (12). https://doi.org/10.1016/S2213-8587(23)00256-5.
Mh, Shah, Goldner Ws, Benson Ab, u. a. 2021. „Neuroendocrine and Adrenal Tumors, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology“. Journal of the National Comprehensive Cancer Network : JNCCN 19 (7). https://doi.org/10.6004/jnccn.2021.0032.
Neumann, Hartmut P. H., William F. Young, und Charis Eng. 2019. „Pheochromocytoma and Paraganglioma“. The New England Journal of Medicine 381 (6): 552–65. https://doi.org/10.1056/NEJMra1806651.
S, Kulkarni, und Wilkinson Ib. 2024. „Adrenoceptors and Hypertension“. Handbook of Experimental Pharmacology 285. https://doi.org/10.1007/164_2024_719.
Tiwari, Rajan Kumar, Shiv Govind Rawat, Siddharth Rai, und Ajay Kumar. 2025. „Stress Regulatory Hormones and Cancer: The Contribution of Epinephrine and Cancer Therapeutic Value of Beta Blockers“. Endocrine 88 (2): 359–86. https://doi.org/10.1007/s12020-025-04161-7.
Y, Zhou, Tai Y, und Shang J. 2025. „Progress in Treatment and Follow-up of Pheochromocytoma“. European Journal of Surgical Oncology : The Journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology 51 (8). https://doi.org/10.1016/j.ejso.2025.110144.
© 2025 EndoCases. All rights reserved.
This platform is intended for medical professionals, particularly endocrinology residents, and is provided for educational purposes only. It supports learning and clinical reasoning but is not a substitute for professional medical advice or patient care. The information is general in nature and should be applied with appropriate clinical judgment and in accordance with local guidelines.
Portions of the text on this website were edited with the assistance of Artificial Intelligence to improve grammar and phrasing, as English is not my first language. All medical content, ideas for illustrations, and overall structure are original and based on the author’s own expertise and the cited medical literature. No AI tools were used to generate or influence the educational content itself.
All of the content is independent of my employer.
Use of this site implies acceptance of our Terms of Use
Contact us via E-Mail: contact@endo-cases.com